Each year, World AIDS Day is held on December 1st to raise awareness about HIV and AIDS. HIV/AIDS still remains a large problem, with nearly 40 million people living with the infection. Hepatitis B (HBV) remains a large issue as well, with 292 million people living with the chronic infection. Despite the inadequate amount of resources or attention that hepatitis B receives, it is important to talk about it whenever we discuss HIV/AIDS. Why? Any individual already living with hepatitis B or HIV can also contract the other infection. This is called a coinfection, and it can have serious consequences if not addressed. Let’s look at HIV/HBV coinfection by the numbers:
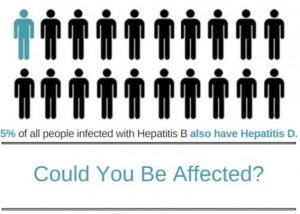
- Globally, 10% of those living with HIV are also living hepatitis B
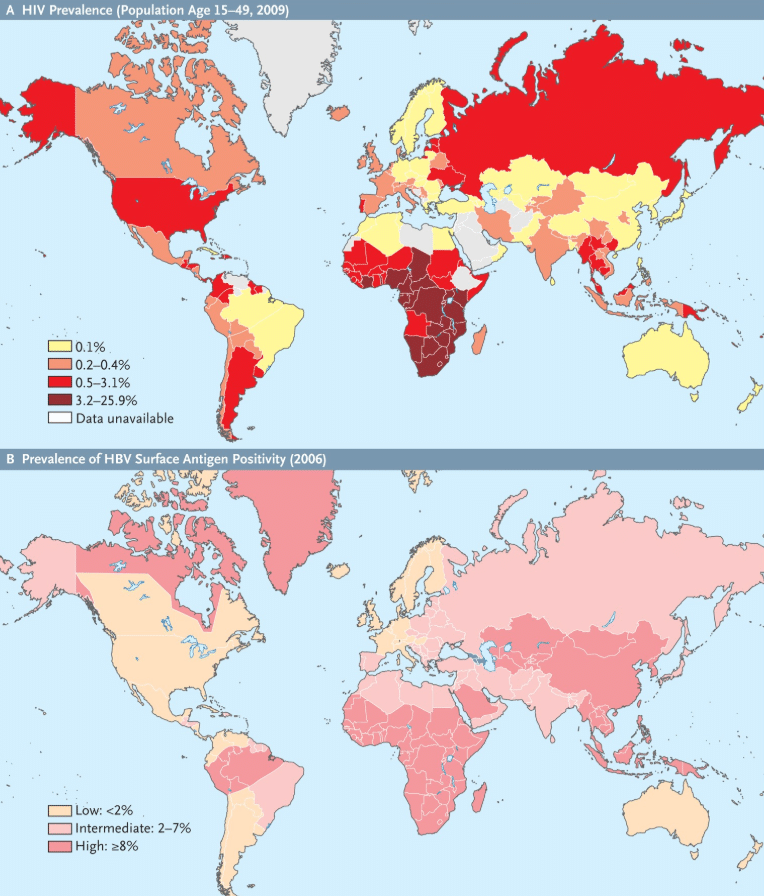
Courtesy of New England Journal of Medicine’s article titled: HIV–HBV Coinfection — A Global Challenge - Coinfection rates can be as high as 25% in countries where both infections are common
- Up to 50% of injection drug users have an HBV/HIV coinfection
- Chronic hepatitis B progression can be up to 5 times faster in coinfected individuals compared to those living with just hepatitis B
HIV vs Hep B: What’s the Difference?
Hepatitis B is a viral infection of the liver that can increase one’s chances of liver disease and liver cancer. HIV is a virus that attacks the immune system and kills the cells that are needed to fight off disease and infection. Though they are two different viruses, they can be spread in similar fashions: direct contact with infected blood, via sexual transmission, injection drug use, and through mother to child transmission during childbirth. Hepatitis B is primarily spread through mother-to-child transmission, HIV is most commonly spread by unprotected sex. Among those living with a coinfection, sexual transmission and injection drug use are the most common modes of transmission. Because of the similar transmission routes, it is recommended that people living with HIV be tested for hepatitis B and hepatitis C and those living with hepatitis B should be tested for HIV.
Hepatitis B may be up to 100 times more infectious than HIV, but it also has a highly effective vaccine! Family members and sexual partners of people living with hepatitis B who have not been infected can protect themselves in just 2 or 3 doses. HIV does not have a vaccine, but people can take precautions to prevent transmission – like not sharing sharp personal items – such as razors, needles, or toothbrushes – and practicing safe sex (use a condom), or through HIV pre-exposure prophylaxis (PRep). Those precautions can also prevent the spread of hepatitis B. While HIV and hepatitis B do not have cures, they both have highly effective treatments. You can learn more about HIV and hepatitis B treatments by clicking the links.
HIV/HBV Coinfection
If you are living with hepatitis B, it is important to get tested for HIV as well. Coinfections are very serious, and can sometimes complicate treatment. Worldwide, HIV/HBV coinfection has become an increased priority because research has shown that conditions associated with hepatitis B and C are now among the leading causes of hospital admission and death in people living with HIV.
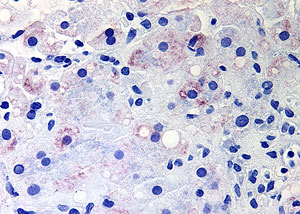
Left untreated and unmanaged, HIV/HBV coinfections can cause rapid progression of liver disease and liver damage, leading to serious complications at younger ages. There is also a higher risk of liver damage from anti-retroviral therapy (HIV treatment) in individuals living with hepatitis B than in those living with just HIV. Though some HIV treatments may also help treat hepatitis B, treatment options can vary based upon the person and the progression of the infections, so it is very important to discuss your options with your healthcare provider. Those living with hepatitis B, HIV, or HIV/HBV coinfection should always be closely monitored by a knowledgeable doctor.
Living with a coinfection can be scary, but with proper management and care, you can lead a healthy life! Check out this video from Jason – one of our #justB storytellers – on successfully living with an HIV/HBV coinfection, and how he has learned to overcome challenges.


 With five different types of viral hepatitis, it can be difficult to understand the differences between them. Some forms of hepatitis get more attention than others, but it is still important to know how they are transmitted, what they do, and the steps that you can take to protect yourself and your liver!
With five different types of viral hepatitis, it can be difficult to understand the differences between them. Some forms of hepatitis get more attention than others, but it is still important to know how they are transmitted, what they do, and the steps that you can take to protect yourself and your liver!  that their primary mode of transmission is through direct blood-to-blood contact with an infected person. Also, both hepatitis B and C can cause chronic, lifelong infections that can lead to serious liver disease. Hepatitis B is most commonly spread from mother-to-child during birth while hepatitis C is more commonly spread through the use of unclean needles used to inject drugs.
that their primary mode of transmission is through direct blood-to-blood contact with an infected person. Also, both hepatitis B and C can cause chronic, lifelong infections that can lead to serious liver disease. Hepatitis B is most commonly spread from mother-to-child during birth while hepatitis C is more commonly spread through the use of unclean needles used to inject drugs.

 By Christine Kukka
By Christine Kukka