On Thursday, Oct. 12, representatives from Hepatitis B Foundation, CDC’s Division of Viral Hepatitis, and NASTAD (the National Alliance of State and Territorial Aids Directors) will co-host a twitter chat at 2 p.m. EST using the hashtag #liverchat.
Also participating is special guest Katherine McGlynn, PhD of the National Cancer Institute. Dr. McGlynn is a Senior Investigator at the National Cancer Institute, Division of Cancer Epidemiology & Genetics, Metabolic Epidemiology Branch. She is a researcher and expert in hepatocellular carcinoma.
Below are questions scheduled to be discussed during the chat. How can you contribute to the conversation? Share any resources or strategies you have that raise awareness and improve liver cancer surveillance. Join the conversation with the hashtag #liverchat.
Q1: What is primary liver cancer and why is raising awareness so important?
Q2: What are the risk factors for liver cancer and why should people with viral hepatitis worry?
Q3: What are some strategies to help prevent viral hepatitis and liver cancer?
Q4: What are the barriers that keep people from getting screened for hepatitis and liver cancer and how can they be addressed?
Q5: What can people living with chronic hepatitis B and C do to protect their liver health and prevent liver cancer?
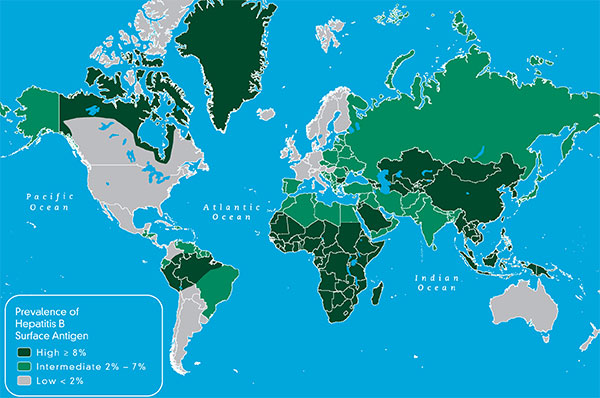
Q6: Why are some populations more vulnerable to viral hepatitis and liver cancer, and how do we address the disparities?
Q7: What can we do to raise awareness & educate vulnerable communities about viral hepatitis and its link to liver cancer?
Q8: What resources are available to learn more about viral hepatitis and liver cancer?
Co-hosts and special guests for the chat include:
- Hepatitis B Foundation – @hepbfoundation
- NASTAD – @NASTAD
- CDC Division of Viral Hepatitis – @cdchep
- CDC Cancer – @cdc_cancer
- Dr. Katherine McGlynn – National Cancer Institute, Division of Cancer Epidemiology and Genetics – @NCIEpiTraining
- CDC National Prevention Information Network (CDCNPIN) will be moderating the chat – @cdcnpin
Confirmed participants and their handles include:
- National Viral Hepatitis Roundtable – @NVHR1
- Hep B United – @hepbunited
- Coalition Against Hepatitis For People of African Origin – @CHIPO_HBV
- Hep B United Philadelphia – @HepBUnitedPhila
- Liver Cancer Connect – @livercancerconn
- Hep Free Hawaii – @hepfreehawaii
- Hep Free NYC – @hepfreenyc
Just getting started with Twitter? Want to know how to join the conversation? Type #liverchat in the search box of the Twitter application to follow the chat, and click on “Latest”.
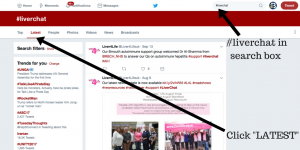
You can prepare your tweets in response to the topics listed above in advance, or you can also tweet on the fly, re-tweet, or Like a tweet from the chat.
The questions are labeled Q1, Q2, etc. so please respond/answer specific question by using A1, A2, etc. in front of your tweets. Remember to include the #liverchat hashtag, which is not case sensitive, in all of your tweets.
If you plan to participate, please contact us at info@hepb.org and we’ll add you to the list of confirmed participants. Let us know if you have any other questions about joining the chat.


 On Wednesday, September 13th, the Multicultural AIDS Coalition – Africans For Improved Access (AFIA) program, Hepatitis B Foundation, and Coalition Against Hepatitis for People of African Origin (CHIPO) commemorated NAIRHHA Day by hosting a webinar discussing “Barriers and Strategies to Addressing HIV and Hepatitis B among African Immigrants: A NAIRHHA Day Webinar.” More than 100 people participated in the webinar. The majority represented government agencies and community-based organizations. This year is particularly exciting because lead organizers also submitted a request to HIV.gov (formerly AIDS.gov) to officially recognize NAIRHHA Day on Sept. 9th as a federal HIV awareness day for African immigrants and refugees in the U.S.
On Wednesday, September 13th, the Multicultural AIDS Coalition – Africans For Improved Access (AFIA) program, Hepatitis B Foundation, and Coalition Against Hepatitis for People of African Origin (CHIPO) commemorated NAIRHHA Day by hosting a webinar discussing “Barriers and Strategies to Addressing HIV and Hepatitis B among African Immigrants: A NAIRHHA Day Webinar.” More than 100 people participated in the webinar. The majority represented government agencies and community-based organizations. This year is particularly exciting because lead organizers also submitted a request to HIV.gov (formerly AIDS.gov) to officially recognize NAIRHHA Day on Sept. 9th as a federal HIV awareness day for African immigrants and refugees in the U.S.