In January of 2020, the Centers for Medicare and Medicaid Services (CMS) proposed a new rule that could increase the out-of-pocket costs for people who take prescription medication for hepatitis B in the U.S. The proposed rule states that health insurance companies would be able to collect patient coinsurance through pharmaceutical manufacturer financial assistance. However, the insurance companies will be allowed to disregard any coinsurance paid with copay assistance when calculating how much the patient has paid toward their deductible and annual out-of-pocket (OOP) limit.
This proposal – titled 2021 Notice of Benefit and Payment Parameters – reverses a recent ruling that would have required health insurance companies to count the value of manufacturer copay assistance toward an enrollee’s annual deductible and OOP limit in most circumstances1. This rule acknowledged that manufacturer copay assistance helps lessen the financial burden of medications for patients. In the US, prescription drugs can be extremely costly, making manufacturer’s copay assistance programs necessary for many patients. For example, brand name treatments are often expensive in order to help pharmaceutical companies earn back the costs of the research and time spent making the medication. Sometimes, the brand name treatments are the only ones that are available, like Vemlidy, or the only version that a person can take. A reversal of the rule would mean that hepatitis B patients and those living with other chronic illnesses may have to pay a larger amount of out-of-pocket costs for their medications.
To understand the significance of this change, we first need to understand what a copay accumulator is.
What is a Copay Accumulator Program and How Does It Work?
A copay accumulator – or accumulator adjustment program – is a strategy used by insurance companies and Pharmacy Benefits Managers (PBMs) that stop manufacturer copay assistance coupons from counting towards two things: 1) the deductible and 2) the maximum out-of-pocket spending. What does this mean?
Previously, a person could receive financial assistance from companies that make a drug, and that would count towards their deductible and/or out-of-pocket costs, depending upon the insurance plan. Pharmaceutical companies often provide financial assistance (such as a co-pay card) to help underinsured individuals afford expensive medications. This means that the person paying for the drug would end up saving money, often thousands of dollars.
Why Is This an Issue?
As the AIDS Institute explains it, “ … the trend in health insurance benefit design is to shift more of the cost of health care to patients through high deductibles and coinsurance rates …In order to afford the medicine they need, patients increasingly rely on manufacturer copay assistance.” With copay accumulators, the individuals who need assistance the most will be unable to receive it, and will end up paying more for their treatments.
Below is an example of a copay accumulator program from the Patient Access Network (PAN) Foundation:
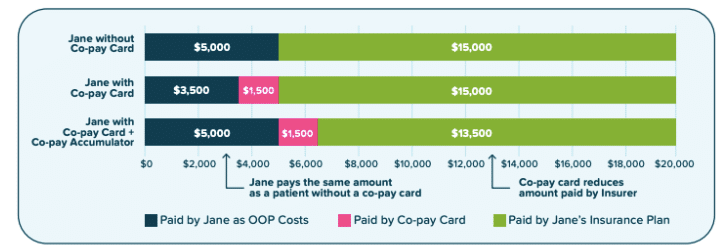
As shown in the above image, with a copay accumulator program – meaning her manufacturer’s assistance is no longer counted toward her out-of-pocket limit- the consumer ends up paying more, while the insurance company is able to reduce the amount they are paying.
Copay accumulator programs are making life-saving treatments increasingly inaccessible. Research shows that the more out-of-pocket costs a person has to pay, the more likely they are to abandon their medication. Once on a hepatitis B medication, stopping suddenly or only taking it once in a while can cause flares and lead to an even higher risk of liver damage.
In the United States, many of those who are living with hepatitis B come from underserved populations with limited access to healthcare. Oftentimes, cultural differences and language barriers can make it difficult to access and utilize the services they need. Now, copay accumulators are making the navigation process even more complex and placing a higher cost burden on patients.
1 The rule required insurance companies to count manufacturer copay assistance toward a patient’s deductible and OOP limit for all brand name drugs for which there is no generic alternative and in cases where the patient gained access to the brand name drug through an insurance plan’s appeals or exceptions process.

