The team at Health Express has voted HBF’s blog as one of the “Must Read Blogs of 2013 – Sexual Health Top 10!” HealthExpress.co.uk is an online clinic that provides support, advice and treatment for common medical conditions that patients do not always feel comfortable talking about. You can take a look at their recommended Top 10 blogs and learn more about them at healthexpress.co.uk.
The team at Health Express has voted HBF’s blog as one of the “Must Read Blogs of 2013 – Sexual Health Top 10!” HealthExpress.co.uk is an online clinic that provides support, advice and treatment for common medical conditions that patients do not always feel comfortable talking about. You can take a look at their recommended Top 10 blogs and learn more about them at healthexpress.co.uk.
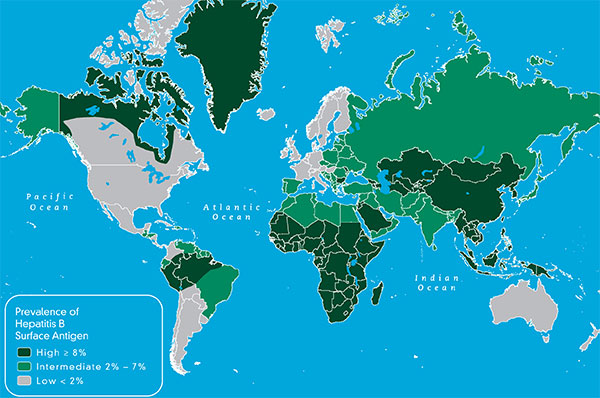
The accolades from the HealthExpress team are a great opportunity to review transmission of the hepatitis B virus. HBV is transmitted through infected blood and body fluids. This includes direct blood-to-blood contact, unprotected sex, unsterile needles, and from an infected woman to her newborn baby at birth. Sharing sharp, personal items that may have trace amounts of blood on them such a razors, toothbrushes, nail clippers and body jewelry including earrings, can also spread the virus. Remember that the HBV virus may live up to a week on a surface resulting in possible transmission through direct blood-to-blood contact. This is why close, household contacts or family members are at greater risk of infection if one or more members are living with HBV. Don’t forget to be sure your tattoo or piercing experience is safe and that the parlor carefully follows infection control practices. Hepatitis B is also 50-100 times more infectious than the HIV virus.
Hepatitis B is also a sexually transmitted disease and is spread through infected semen, vaginal fluids and any blood that may be exchanged as part of a sexual practice – most often through sexual intercourse. In the United States, sexual transmission is the most common mode of HBV transmission and is responsible for 2/3 of acute HBV infections. A common question is “what about oral sex?” In general, oral sex would be considered less risky, but any kind of intimate sharing that may result in the exchange of bodily fluids will present some degree of risk.
So how can you prevent hepatitis B transmission between sexual partners? Fortunately there is a safe and effective hepatitis B vaccine to protect against the spread of HBV. Get screened for HBV and vaccinate to protect – especially if you or your partner has more than one sexual partner, or if one or more partners is at greater risk. When in doubt, get screened. Keep in mind that HBV is referred to as a “silent infection” since it may take decades for symptoms to occur. People with chronic HBV may be completely unaware of their infection and inadvertently spread HBV to their partner(s) if precautions are not taken.
Other precautions include practicing safe sex by using a latex or polyurethane condom. A lambskin condom will not prevent the spread of hepatitis B or other viral STDs. Looking for condom details?
A general comment to those with multiple sex partners– We are very fortunate to have a vaccine to protect against the hepatitis B virus. However, practicing safe sex with an effective condom is always advised to prevent the transmission of other infectious diseases that are not vaccine preventable, such as HCV and HIV, along with condom use to prevent the spread of other sexually transmitted diseases. Use common sense. No one wants a sexually transmitted disease, and if you have HBV, you really don’t want a coinfection. It can really complicate your life.