
Hepatitis B remains a global health challenge.. There are strategies to prevent perinatal (mother to child) transmission of hepatitis B. Prevention includes testing all pregnant persons for the marker of hepatitis B infection (HBsAg), if the pregnant person is positive, then assessment is needed throughout pregnancy. If the pregnant person’s viral load becomes high, antiviral treatment (TDF) might be recommended during the second trimester taken throughout pregnancy. Data shows this is safe and effective, and reducing the viral load can reduce the risk of transmission.
Additionally, making sure that all infants get hepatitis B birth dose as soon as possible after delivery, ideally within the first 24 hours of birth followed by at least two subsequent doses of hepatitis B vaccine (usually part of global childhood immunization series ex: the pentavalent vaccination). However, for many individuals, adhering to these guidelines in many parts of the world can be a challenge. Recent research sheds light on the barriers and opportunities to improve treatment adherence during this important period. Treatment adherence means taking your medicine the right way, at the right time, in the right amount, and for as long as your doctor tells you. It’s about sticking to your treatment plan to maintain your health.
The postpartum drop-off: a hidden risk
A study published in the Journal of the Pediatric Infectious Diseases Society explored adherence to tenofovir disoproxil fumarate (TDF), a medication used to treat HBV, among pregnant individuals. While adherence during pregnancy was relatively high, many women discontinued treatment postpartum. A mix of factors contributed to the drop in HBV treatment adherence following delivery including:
- Lack of follow-up care after delivery
- Low awareness about health risks that may come from stopping medication
- Limited knowledge about the long-term benefits of continued treatment
- Healthcare system gaps, especially in low-resource settings, making access to care and medication difficult
What the numbers say?
In a broader context, a study from Israel found that only about 67% of chronic HBV patients maintained high adherence (defined as taking at least 80% of the prescribed medication). Many women stopped taking their medication after giving birth or were not consistent with their medication routines (Mor et al., 2022). A 2025 pilot study published in Virology Journal looked at what happens when women with chronic hepatitis B stop taking antiviral medication after giving birth. Among 88 women who discontinued treatment postpartum, nearly 29% experienced liver inflammation (ALT flares)—a sign that the virus was becoming elevated (Tang et al., 2025).
What can be done?
Improving postpartum adherence to HBV treatment requires a holistic approach and strategies can include:
- Integrated care models that link obstetric and hepatology services, making it easier for women to stay on track with their hepatitis B care and medication
- Patient education that emphasizes the importance of continued treatment beyond pregnancy
- Support from community health workers to provide follow-up and encouragement to stay connected with hepatitis B care
- Mobile health tools (like SMS reminders) to help new mothers stay on track after delivery
The postpartum period is a time of immense change—and often, medical follow-up takes a backseat. But for women living with HBV, taking efforts to prevent perinatal transmission is crucial not just for their own health, but for preventing the future generation from hepatitis B. With better systems, education, and support, we can close the adherence gap and protect more lives.
To learn more about prevention of perinatal transmission of hepatitis B, you can also visit the Hepatitis B Foundation’s Informed Training Hub, which includes modules on perinatal prevention.
References:
Greenup, A. J., Tan, J., Nguyen, V., & Visvanathan, K. (2020). Adherence to antiviral therapy for chronic hepatitis B during pregnancy and postpartum: A prospective cohort study. Journal of the Pediatric Infectious Diseases Society, 9(3), 289–295. https://doi.org/10.1093/jpids/piz064
Mor, Z., Grotto, I., & Anis, E. (2022). Adherence to antiviral therapy among patients with chronic hepatitis B in Israel. Israel Journal of Health Policy Research, 11(1), 1–9. https://doi.org/10.1186/s13584-022-00527-2
Tang, Q., Wang, C., Li, H., Chen, Z., Zhang, L., Zhang, J., Liu, X., Xue, Y., Qiu, Y., Peng, M., Zeng, Y., & Hu, P. (2025). Unexpected HBsAg decrease after nucleoside analogues retreatment among HBeAg positive postpartum women: A pilot study. Virology Journal, 22, Article 36. https://doi.org/10.1186/s12985-025-02632-x
World Health Organization. (2024). Guidelines for the prevention, diagnosis, care and treatment for people with chronic hepatitis B infection (WHO Guidelines). https://www.who.int/publications/i/item/9789240090903


 Around the world, the most common mode of hepatitis B transmission is from mother to child. Unfortunately, pregnant mothers who have hepatitis B can transmit the virus to their newborn during the delivery process. 90% of these HBV infected babies will progress to chronic infection putting them at increased risk of serious liver disease or liver cancer later in life.
Around the world, the most common mode of hepatitis B transmission is from mother to child. Unfortunately, pregnant mothers who have hepatitis B can transmit the virus to their newborn during the delivery process. 90% of these HBV infected babies will progress to chronic infection putting them at increased risk of serious liver disease or liver cancer later in life.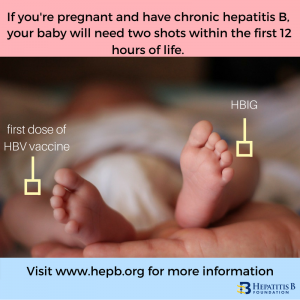 The
The 
