As of 2019, the Centers for Disease Control and Prevention (CDC) requires over 100 diseases, infections and conditions – including hepatitis A, B and C – to be reported by state and local health departments. Physicians who diagnose these conditions, and diagnostic laboratories, are required to report confirmed and/or suspected cases to health departments, who then notify the CDC. This requirement allows the government to monitor disease patterns and track outbreaks to contain the spread of disease and protect the public. While all other forms of viral hepatitis are federally ‘reportable’, hepatitis delta cases are not required to be reported. Hepatitis delta is the most severe form of viral hepatitis, and spreads similarly to hepatitis B; through blood and sexual fluids, making it a public health threat, particularly for the 2.2 million people who already have hepatitis B in the U.S.
Hepatitis delta can only be contracted along with hepatitis B or after someone is already infected with hepatitis B. Acute cases can cause liver damage and even liver failure, and in chronic cases, can accelerate the rate of liver disease progression, as there are no effective treatments available. Although estimated to affect 5-10% of hepatitis B patients, hepatitis delta is severely underdiagnosed, leaving the true disease burden largely unknown in the U.S. and worldwide.
In conjunction with awareness efforts, adding hepatitis delta as a reportable disease could reveal a more accurate prevalence landscape of hepatitis B and delta coinfection and allow for more effective prevention efforts. The CDC asserts that “reporting of cases of infectious diseases and related conditions has been and remains a vital step in controlling and preventing the spread of communicable diseases,1” yet hepatitis delta has still been left out of the list of nationally reportable diseases. While notifying CDC is only voluntary2, 23 states have designated hepatitis delta infections as reportable to local and state health departments, allowing for surveillance of outbreaks, particularly relevant to the current nationwide opioid crisis.
Worchester, Massachusetts, which is currently experiencing a hepatitis A outbreak, also saw one of the worst hepatitis delta outbreaks in the country in the mid 1980’s. The infection was seen among drug users and their sexual partners, sickened 135 people, and killed 15. In those infected with hepatitis B, delta coinfection was present in 54% of drug users and 33% of their sexual partners3
. Interestingly, in Massachusetts, only labs (and not clinicians) are required to report hepatitis delta cases. The reporting requirement allowed the state to be alerted of a spike in cases and respond accordingly – a luxury many other states may not have if neither labs nor clinicians are required to report in their state.
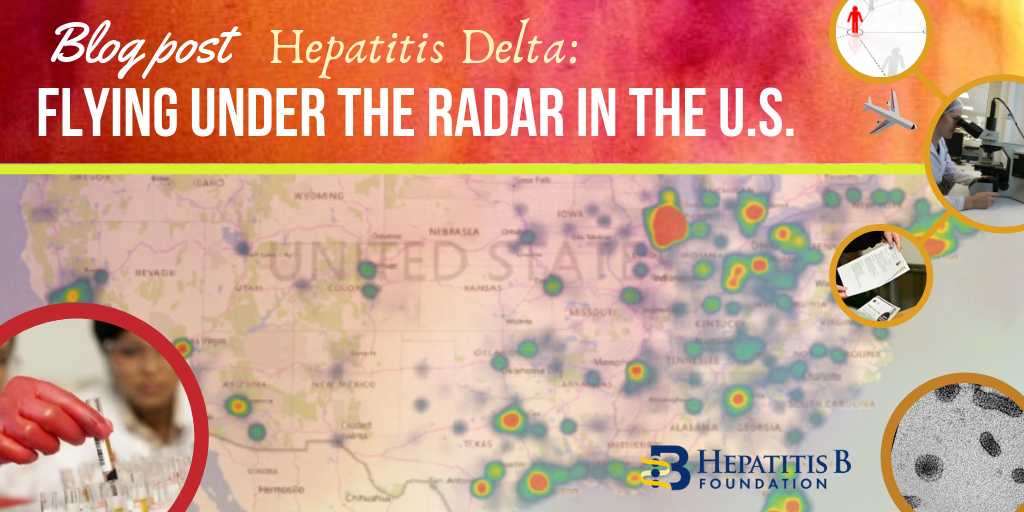
Some states are even scaling back their surveillance; in 2016, New York State removed hepatitis delta from their list of reportable diseases, citing just 21 cases in a two-year period and a health code that asserts a “providers obligation” to “report unusual manifestations of novel strains of hepatitis.”4. Although hepatitis delta is more common outside the U.S., there is evidence to suggest persistent and even growing prevalence. A 2016 prevalence map presented by Eiger BioPharmaceuticals revealed New York City as a “hot-spot” for hepatitis delta cases5. Although more recent prevalence studies are sparse, and often include only small sample sizes, several have noted increases in hepatitis delta coinfection among certain groups. One study in Baltimore, published in 2010, compared blood samples from drug users in the 1980’s to samples obtained from 2005-2006 – and found a 21% increase in hepatitis delta coinfection among people already chronically infected with hepatitis B6. A 2015 study analyzed the blood records of 2,100 hepatitis B positive veterans – nearly 4% were coinfected7. A larger study, analyzing chart records of 500 chronic hepatitis B patients in California found that 8% of patients had a delta coinfection8. Another 2018 publication utilized data from 2011-2016 from the National Health and Nutrition Examination Survey (NHANES) and estimated there to be over 350,000 Americans with past or current hepatitis delta9.
While the true burden of hepatitis delta in the U.S. is debated, one study that analyzed diagnosis codes for over 170 million people showed 10,000 coinfected patients newly diagnosed in 2016 alone4. The American Association for the Study of Liver Diseases (AASLD) recommends delta testing in high-risk groups, but countless journals and leading hepatologists have called for universal testing of hepatitis B patients for hepatitis delta9,10,11 which could reveal thousands of unknown infections. Low awareness, testing, and the lack of inclusion on the notifiable diseases list contribute to the unclear picture of prevalence in the U.S. Inconsistent reporting across states creates holes in data collection and opportunities for missed outbreaks and subsequent treatment and prevention efforts. Adding hepatitis delta to the list of reportable diseases nationally could be the key to understanding who this ‘hidden epidemic’ is affecting, and where, and allow for effective surveillance to prevent future infections.
For more information about Hepatitis Delta Connect or hepatitis delta, visit www.hepdconnect.org or email connect@hepdconnect.org.
References:
1. Centers for Disease Control and Prevention. (1990, June 22). Mandatory Reporting of Infectious Diseases by Clinicians. Morbidity and Mortality Weekly Reports. Retrieved from https://www.cdc.gov/mmwr/preview/mmwrhtml/00001665.htm.
2. Centers for Disease Control and Prevention. (2018). National notifiable diseases surveillance system (NNDS): Data collection and reporting. Retrieved from https://wwwn.cdc.gov/nndss/data-collection.html
3. Lettau, L. A., McCarthy, J. G., Smith, M. H., Hauler, S. C., Morse, L. J., Ukena, T., et al. (1987). Outbreak of severe hepatitis due to delta and hepatitis B viruses in parenteral drug abusers and their contacts. N Engl J Med, 317(20), 1256-1262.
4. The City of New York. (2016). Hepatitis D and E and other suspected infectious viral hepatitides reporting. Retrieved from http://rules.cityofnewyork.us/tags/reportable-diseases.
5. Martins, E and Glenn, J. Prevalence of Hepatitis Delta Virus (HDV) Infection in the United States: Results from an ICD-10 Review. Poster Sa1486 DDW May 2017.
6. Lauren M. Kucirka, Homayoon Farzadegan, Jordan J. Feld, Shruti H. Mehta, Mark Winters, Jeffrey S. Glenn, Gregory D. Kirk, Dorry L. Segev, Kenrad E. Nelson, Morgan Marks, Theo Heller, Elizabeth T. Golub, Prevalence, Correlates, and Viral Dynamics of Hepatitis Delta among Injection Drug Users, The Journal of Infectious Diseases, Volume 202, Issue 6, 15 September 2010, Pages 845–852.
7. Kushner, T., Serper, M., & Kaplan, D. E. (2015). Delta hepatitis within the veterans affairs medical system in the United States: Prevalence, risk factors, and outcomes.
8. Gish, Robert & Yi, Debbie & Kane, Steve & Clark, Margaret & Mangahas, Michael & Baqai, Sumbella & A Winters, Mark & Proudfoot, James & Glenn, Jeffrey. (2013). Coinfection with Hepatitis B and D: Epidemiology, Prevalence and Disease in Patients in Northern California. Journal of gastroenterology and hepatology. 28. 10.1111/jgh.12217
 America to help raise money and awareness for hepatitis B research, patient outreach, and education through the Hepatitis B Foundation! You can make a gift to support Edwin’s fundraising efforts here.
America to help raise money and awareness for hepatitis B research, patient outreach, and education through the Hepatitis B Foundation! You can make a gift to support Edwin’s fundraising efforts here. Triathlon in Minnetonka, Minnesota – his first of six races this summer. In just under an hour and a half he accomplished: swimming more than 100 yards, biking 15 miles, and running 3 miles!
Triathlon in Minnetonka, Minnesota – his first of six races this summer. In just under an hour and a half he accomplished: swimming more than 100 yards, biking 15 miles, and running 3 miles!




 NORD through participating in rare disease Twitter chats and presenting a poster at the NORD Rare Action Summit in October 2018. We’re very excited to be a part of the coalition, and to be spreading awareness about hepatitis delta!
NORD through participating in rare disease Twitter chats and presenting a poster at the NORD Rare Action Summit in October 2018. We’re very excited to be a part of the coalition, and to be spreading awareness about hepatitis delta!
 with hepatitis B could take a physical and mental toll on an individual and impact how they viewed themselves. Edwin’s observations inspired him to reach out to the Hepatitis B Foundation to
with hepatitis B could take a physical and mental toll on an individual and impact how they viewed themselves. Edwin’s observations inspired him to reach out to the Hepatitis B Foundation to
 The nail salon industry is regulated at the state level by a regulatory Board of Cosmetology that oversees and ensures nail technicians and nail salons comply with all rules and regulations. In this report, we analyze the nail salon workforce and industry regulations and provide recommendations that can address specific concerns. We conducted phone interviews with health clinics, public health workers, and other relevant stakeholders to better understand the challenges this population encounters when accessing hepatitis B education and care. In addition, we conducted a policy analysis of each state’s Board of Cosmetology to assess their effectiveness in protecting workers from exposure to bloodborne pathogens, specifically hepatitis B. In our analysis, we found that several states may not adequately protect workers from workplace hazards that may increase their risk of hepatitis B exposure. With sanitation and disinfection requirements that greatly vary between states, low compliance can leave workers susceptible to the transmission of bloodborne pathogens, including the hepatitis B virus.
The nail salon industry is regulated at the state level by a regulatory Board of Cosmetology that oversees and ensures nail technicians and nail salons comply with all rules and regulations. In this report, we analyze the nail salon workforce and industry regulations and provide recommendations that can address specific concerns. We conducted phone interviews with health clinics, public health workers, and other relevant stakeholders to better understand the challenges this population encounters when accessing hepatitis B education and care. In addition, we conducted a policy analysis of each state’s Board of Cosmetology to assess their effectiveness in protecting workers from exposure to bloodborne pathogens, specifically hepatitis B. In our analysis, we found that several states may not adequately protect workers from workplace hazards that may increase their risk of hepatitis B exposure. With sanitation and disinfection requirements that greatly vary between states, low compliance can leave workers susceptible to the transmission of bloodborne pathogens, including the hepatitis B virus.
 Join
Join