
I thought hepatitis B was sexually transmitted? I just tested positive, but my partner tested negative, we’ve been together for years, what gives?
This question is a common one. Hepatitis B can be transmitted sexually, so why do some people — who were not vaccinated — never get hepatitis B from their sexual partners?
It comes down to factors, such as the type of sexual activity partners engage in, the viral load (HBV DNA) of the infected partner, and who is on the receiving end of infectious body fluids, especially blood (which contains the most virus), and semen.
Having one partner infected, while the other is not, can add more stress to an already traumatic hepatitis B diagnosis. “It was very confusing and made me question how was it possible I was the only one infected,” said a woman who tested positive while her husband tested negative. “I thought it was possibly a mistake, maybe I was a biological anomaly, which of course I was not.”
Let’s look at the factors that may play a role in transmission of hepatitis B infection through sexual activity.
Viral load: Semen, vaginal fluids and blood all contain the hepatitis B virus (HBV), and the higher the viral load in the blood of an infected individual, the more infectious they are considered to be. Having an undetectable viral load might reduce or eliminate the chance of transmitting the virus to someone during unprotected sex; research is still trying to assess whether a person with an undetectable viral load in the blood is able to transmit the virus through sex. This is a good reason for individuals living with hepatitis B to talk to their doctor about the benefits of starting antivirals if they have detectable HBV viral load in their blood; treatment which lowers the viral load in the blood might also serve as a prevention measure for transmitting the virus.
Once an individual tests positive for hepatitis B surface antigen (HBsAg), they should encourage their partners to get screened for hepatitis B, and vaccinated if they are still susceptible to the virus.
The timing of sexual activity: An infected person who is menstruating is more likely to transmit hepatitis B infection to an unvaccinated partner, because menstrual blood can contain higher levels of HBV than vaginal secretions. That is why dental dams and condoms are recommended to provide a reasonable barrier against exposure, during that time of the month.
The type of sexual activity: Certain sexual activities are far more efficient at transmitting hepatitis B virus than others. Oral sex appears to have a lower rate of hepatitis B transmission than vaginal sex. Anal sex carries a higher risk of transmission because of tears in the skin that can occur during penetration, which increases the likelihood of transmission of HBV to an unvaccinated partner.
Fingering carries a lesser risk, unless the infected partner is menstruating while the other partner has bruises or cuts on their hands that could allow entry of hepatitis B virus from the body fluid into the bloodstream. In such cases, gloves are highly recommended.
The hepatitis B status of the other partner: The “uninfected” partner could have already been infected and cleared the virus, or vaccinated as an infant. When a person is first diagnosed with hepatitis B, doctors often test his or her partner for only the hepatitis B surface antigen (HBsAg), which indicates a current hepatitis B infection. If they are negative for HBsAg, they are advised to receive the hepatitis B vaccine as soon as possible. However, this does not mean that they were never infected.
Testing for the hepatitis B surface antibody (also known as anti-HBs or HBsAb), and hepatitis B core antibody (HBcAb) is the only way to identify a past recovered infection or prior vaccination.
Hepatitis B is often called the “silent” infection because many people who get hepatitis B may not experience any of the alarming symptoms (like fever or jaundice). As a result, many individuals may never realize they were infected. A partner who tested negative for HBsAg, may actually have been infected in the past and cleared the infection and now has protective hepatitis B surface antibodies to forever safeguard them from infection. If they’re vaccinated without proper screening, then tested for HBsAb after vaccination, they will test positive for surface antibodies, without ever knowing that their antibodies resulted from a past infection, not immunization.
Bottom line, if one partner is diagnosed with hepatitis B and the other is not, it might seem unusual, but it is not uncommon. Just like any other virus, there is not a 100% chance of transmission with exposure. The undiagnosed partner should get tested using the 3-panel blood test (HBsAg, HBsAb, and HBcAb) and immediately vaccinated if they are still vulnerable to a hepatitis B infection (HBsAb negative).
The is safe, effective, and provides lifelong protection.
Take a quiz to find out how much you know about hepatitis B transmission: click here.





 March 27th is
March 27th is  Around the world, the most common mode of hepatitis B transmission is from mother to child. Unfortunately, pregnant mothers who have hepatitis B can transmit the virus to their newborn during the delivery process. 90% of these HBV infected babies will progress to chronic infection putting them at increased risk of serious liver disease or liver cancer later in life.
Around the world, the most common mode of hepatitis B transmission is from mother to child. Unfortunately, pregnant mothers who have hepatitis B can transmit the virus to their newborn during the delivery process. 90% of these HBV infected babies will progress to chronic infection putting them at increased risk of serious liver disease or liver cancer later in life.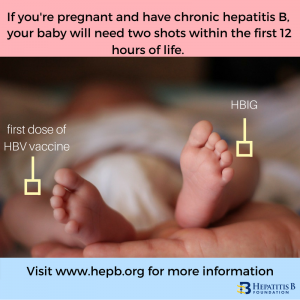 The
The  Around the world, millions of people with chronic hepatitis B face wrenching discrimination that limits their dreams, education, careers, income and personal relationships.
Around the world, millions of people with chronic hepatitis B face wrenching discrimination that limits their dreams, education, careers, income and personal relationships.
