
April is Alcohol Awareness Month!
Hepatitis B is a virus that can damage the liver. The liver is a critical organ in the human body and is responsible for energizing cells, removing toxins and waste, and strengthening the immune system. It is most commonly understood as the body’s primary filtering system and storage unit. Alcohol consumption has been shown to cause serious problems for the liver as it overwhelms the liver’s ability to carry out important tasks.
Important Functions of the Liver:
Bile Production: Bile is a greenish liquid released from the liver and into the gallbladder (a small sac located under the liver which stores bile) that helps to break down fats so they can be used by the body. The liver produces and cleans bile so that it can move through the small intestine. Bile also helps to remove some toxins and waste products such as excess cholesterol (a type of fat necessary for digestion and healthy cells) and bilirubin (a yellow substance made from old red blood cells) to keep your immune system healthy and clean. Even though cholesterol is an important substance, excess amounts of cholesterol can clog the bloodstream and cause serious problems like heart disease. This is why the liver removes unwanted cholesterol from the body. Similarly, bilirubin is made during the production of bile and is a waste product of old and broken-down red blood cells. A healthy liver can filter out and remove bilirubin from the body. High amounts of bilirubin may indicate damage to the liver or serious liver disease.
Natural Detoxification: The liver is most notably known for its natural detox system, which is one of its most important functions. The liver removes toxins, foreign substances, and harmful waste from the bloodstream such as alcohol, drugs, and other chemicals through different ways. Depending on the substance, it may remove the toxin through bile, break it down into safer substances so the toxins don’t cause harm. The liver can even store the toxins, so the rest of the body is safe. It is important to understand that, even though the liver has a remarkable filtering system, it has limits and should not be put under excess stress.
Blood Glucose Regulation: Glucose is a sugar molecule and the most important source of energy for your body. Glucose enters the body through foods high in carbohydrates, such as grains, potatoes and fruits. During the digestive process, glucose molecules from foods are broken down and used by the body to energize cells and maintain the most basic yet critical functions of the immune system. Glucose turns into blood glucose or blood sugar when it travels through the bloodstream. For glucose to be used as energy by the cells, it needs assistance from insulin (a hormone released by the pancreas), which helps it move around and get to the cells. Think of insulin as the key and glucose as the lock. The key opens the lock to the door. Similarly, insulin opens the door so that glucose can get inside the cells and provide energy. High levels of blood glucose and the inability to produce or use insulin properly can result in diabetes. Even though glucose comes from food, the human body can use the liver to produce its own glucose. The liver is basically the storage unit for glucose, saving it for use at a later time in the form of glycogen. Glycogen or stored glucose is released on an “as– needed basis.” When the body is running low on glucose, the liver uses fats to provide energy and saves the remainder of the glucose for the most important organs that need sugar for energy, such as the brain and kidneys.
Alcohol Consumption and the Liver:
Alcohol is a toxic substance and is known to cause a powerful effect on the brain’s ability to understand and process information because the brain is a very sensitive organ. This is why alcohol can be so addictive for some people. It causes chemical effects (excess release of dopamine, a hormone that makes you feel good) in the brain, which can lead to addiction. Increased intake of alcohol is also linked to several health issues such as cancer, heart disease, digestive problems and liver disease. Alcohol use is also associated with injuries such as fatal car crashes and alcohol overdose.
Since the liver is the body’s natural detox system, alcohol consumption disrupts the liver from carrying out its most important tasks. For example, the liver’s role is to remove alcohol from the blood. Breaking down ethanol (found in alcohol) causes some liver cells to die. The liver is able to make new cells but too much alcohol or long-term use can reduce the ability to make repairs. The U.S. Centers for Disease Control and Prevention (CDC) defines more than two drinks per day for men and one drink per day for women to be excessive alcohol use. Drinking too much inflames the liver and disrupts its filtering system. Damaged and weakened liver cells are unable to remove the toxins from alcohol from the blood. When liver cells are destroyed, they are unable to carry out the other important tasks such as producing bile, making proteins and storing glucose.
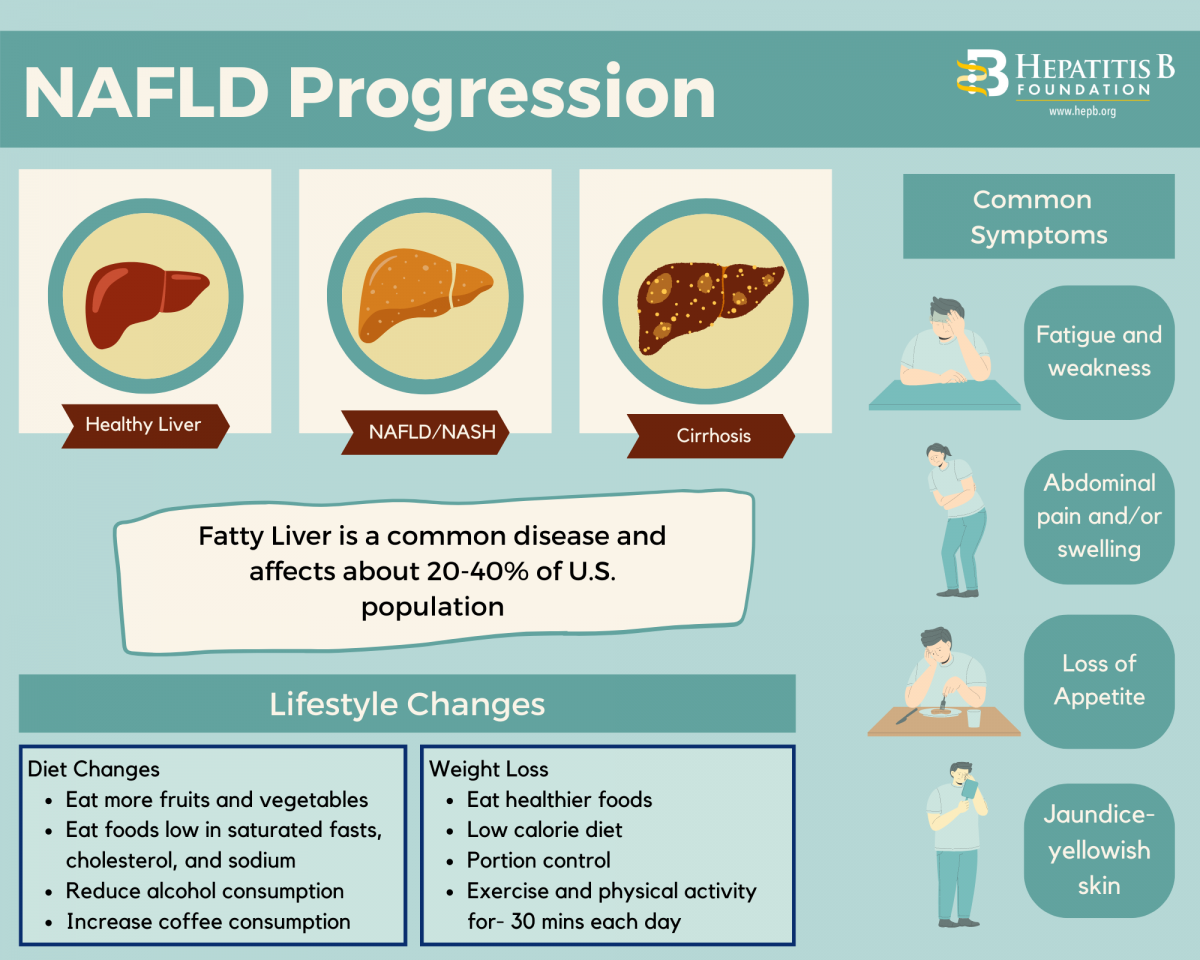
The most common type of alcohol– related disease is fatty liver. This is when excess amounts of fat are found in the liver. This causes the liver to swell, and overtime may cause inflammation or cirrhosis (scarring of the liver). Any damage to the liver cells, whether it’s through swelling, inflammation, or scarring, disrupts the liver’s ability to carry out its most essential functions. Cirrhosis or scarring of the liver is the most dangerous thing that can happen to the liver. It means that healthy liver tissue and cells are now being replaced by scar tissue from liver damage. The symptoms of liver damage from alcohol use may consist of fever, vomiting, nausea, jaundice, abdominal pain, fatigue and loss of appetite. This process is not sudden and usually takes a long time to happen. However, symptoms and signs may not always be present.
What People Living with Hepatitis B Should Know About Drinking Alcohol?
People living with hepatitis B should know that the liver is already weakened by the virus. The hepatitis B virus attacks the healthy liver cells and tissue and causes inflammation. Alcohol use can result in more problems and can put greater stress on the liver. It can speed up the harm to the liver, resulting in serious liver disease. It can lower the body’s ability to defend itself from foreign invaders, such as other viruses and bacteria. Studies have shown that alcohol intake can result in rapid HBV replication, further increasing the risk of cirrhosis and liver disease.
Love your Liver!
In a recently published statement by the World Health Organization, it was found that “no amount of alcohol is safe when it comes to health.” It is important to understand that alcohol, whether little or much, is a toxin and puts the liver at the highest risk as the liver is the natural detox for unwanted and harmful substances. The liver does a lot to keep our bodies protected from harm and acts as a natural defense. But, like people, the liver can also experience burnout. It is very important to keep our liver healthy, safe, and away from harm!
References:
https://www.hopkinsmedicine.org/health/conditions-and-diseases/alcoholinduced-liver-disease
https://www.verywellhealth.com/definition-of-bile-1759867
https://www.ncbi.nlm.nih.gov/books/NBK470209/
http://hepctrust.org.uk/information/liver/detoxification







 Both issues can impair the liver’s ability to function and filter out toxins that enter the body. They can also increase a person’s risk of developing liver cancer. Recently,
Both issues can impair the liver’s ability to function and filter out toxins that enter the body. They can also increase a person’s risk of developing liver cancer. Recently,