Happy Hepatitis Awareness Month! Continue reading to get to know the Viral Hepatitis Program at the Philadelphia Department of Public Health (PDPH)!
The Viral Hepatitis Program at PDPH strives to support Philadelphia residents and service providers in several ways, including preventing viral hepatitis infection through education, screening, and vaccination; improving and providing access to affordable treatment; and supporting provider efforts to provide comprehensive viral hepatitis care/treatment. There are many tools that exist to prevent and treat viral hepatitis infections, and even cure them in the case of hepatitis C. Access to these services, however, is not readily available for everyone. The Viral Hepatitis Program aims to increase access and reduce inequities in care through collaborations and programming, in hopes of achieving the 2030 goal of hepatitis B and hepatitis C elimination.
The Viral Hepatitis Program performs a number of exciting projects to achieve this work!

Patient Engagement
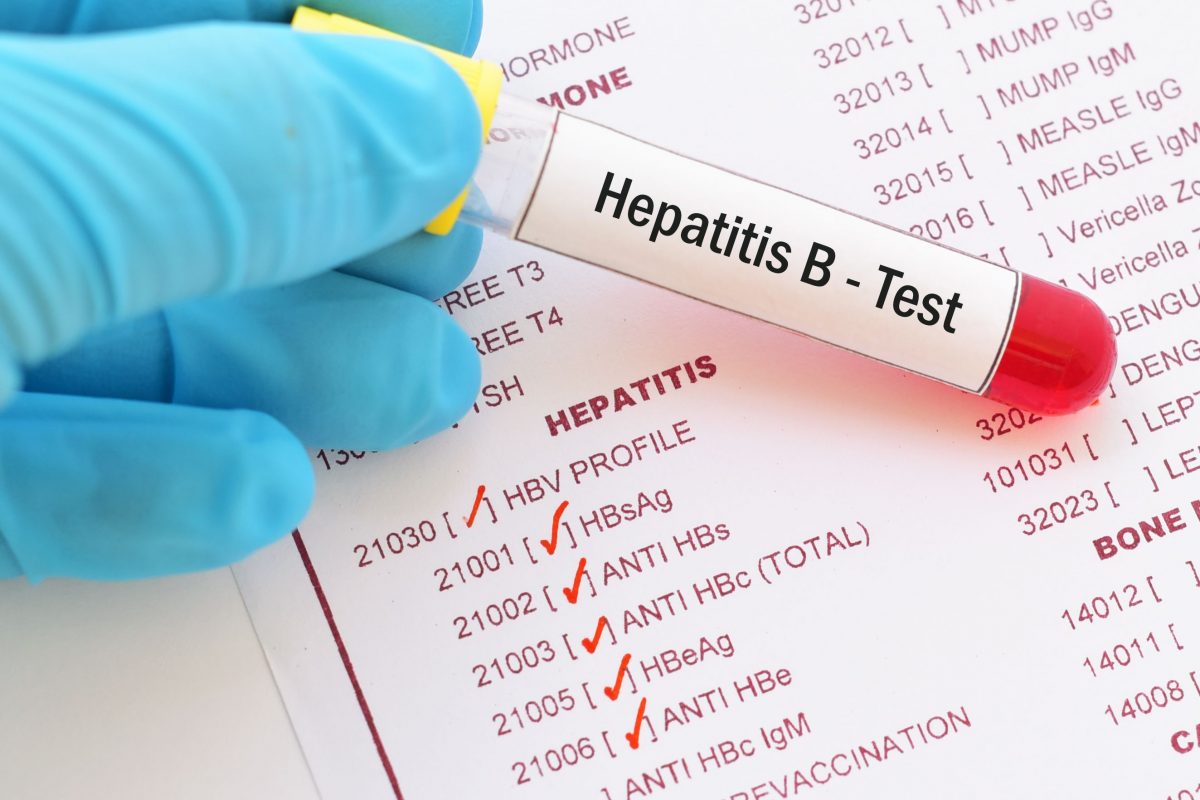
Many members of the Viral Hepatitis Program spend their days interacting with patients over the phone. Public health surveillance allows the program to work with hepatitis B and hepatitis C patients to provide individualized support. This outreach provides patients with viral hepatitis education, linkage-to-care, and care navigation along with access to harm reduction materials, support for substance use disorder care, and additional resources.
Above: Viral Hepatitis team member, Cassandra Lamadieu, provides viral hepatitis educational materials to community members in attendance at the 2023 Philadelphia Block Captain Rally.
Philly InSync: Provider Engagement
Through collaborations within PDPH and with a partner organization, the Philly InSync Project provides education and technical assistance to healthcare providers and facilities to integrate harm reduction, substance use disorder care, and care for infectious diseases related to drug use. Philly InSync works with multiple sites to provide testing, care, and treatment of hepatitis B, hepatitis C and other infectious disease care while also providing technical assistance including staff trainings, data improvement strategies, and reducing barriers to care. A technical advisory committee of Philadelphia providers meets quarterly to provide enhanced technical assistance to these sites while learning how to improve the care they provide as well. The program elevates conversations among Philadelphia providers and creates a collaborative community to learn, listen, and share experiences, challenges, and solutions that involve anything from clinical experiences to insurance barriers.
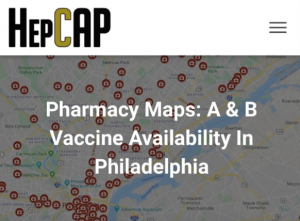
Pharmacy Project: Increasing Hepatitis A & B Vaccination
Another project to increase viral hepatitis prevention efforts is the Pharmacy Project, which is focused on improving pharmacy-based vaccination for hepatitis A & B. Annually, the Viral Hepatitis Program conducts a survey of pharmacies in Philadelphia to collect information about hepatitis A and B vaccination services. The survey results are shared with the community on a map that allows patients and providers to find vaccinating pharmacies. The data collected is also used to identify barriers to vaccine access, to inform additional activities to support patients, providers, and pharmacists.
Social Media
To engage the community and to promote collaboration, the program runs several social media accounts and provides up-to-date information and resources. To access information on vaccine events, mobile health clinics, and many other health services follow along at the links below! Make sure to follow along during the month of May for some special Hepatitis Awareness Month content!

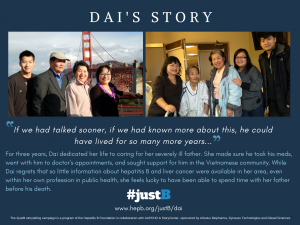
Philadelphia Hepatitis B & Hepatitis C Elimination Plan
The Viral Hepatitis Program and local partners and community members have worked together to create a plan for the elimination of hepatitis B and hepatitis C in Philadelphia. To see information on this process visit: Philadelphia Hepatitis B & Hepatitis C Elimination Plan Community Engagement Executive Summary. Striving to eliminate the impact of these infections from Philadelphia is not a new effort, as a committed community of viral hepatitis eliminators has been hard at work for quite some time. Hep B United – Philadelphia and The Hepatitis C Allies of Philadelphia (HepCAP) are the two local coalitions made up of individuals and organizations committed to viral hepatitis elimination. While much has been accomplished, PDPH and the local community of eliminators are continuing the work to provide services to educate, prevent, vaccinate, test, link-to-care, and treat these two diseases in Philadelphia. The Plan will be released in 2023.
To learn more about viral hepatitis or for any questions…
Websites: Phillyhepatitis.org & Hepcap.org
Email: hep-ddc@phila.gov
To order educational materials: bit.ly/hepeducationalmaterials










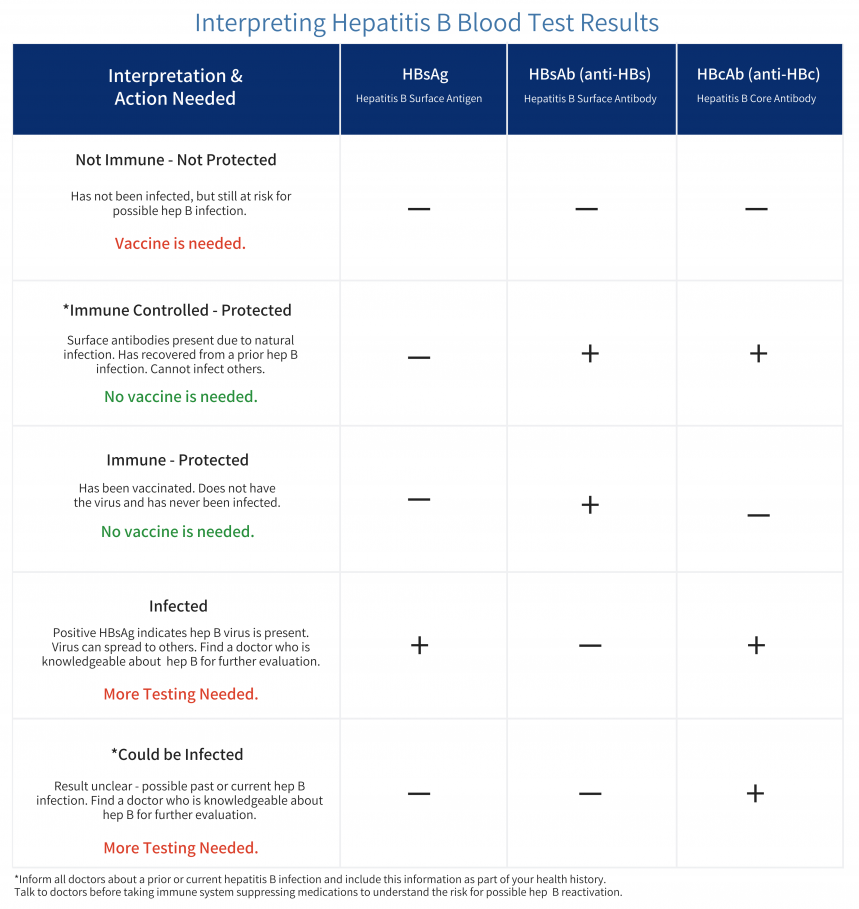
 Yufei Zhao is 45 years old and lives with his family in Philadelphia, Pa. Yufei discovered that he had hepatitis B when he attended a community health fair with his family. Even though he was instructed to talk about his diagnosis with a doctor and learn more about possible treatment options, Yufei decided to do nothing as he did not feel sick. While he has health insurance through his employer, he never utilizes any health care services. He often skips annual wellness visits as he says he “never gets sick.”
Yufei Zhao is 45 years old and lives with his family in Philadelphia, Pa. Yufei discovered that he had hepatitis B when he attended a community health fair with his family. Even though he was instructed to talk about his diagnosis with a doctor and learn more about possible treatment options, Yufei decided to do nothing as he did not feel sick. While he has health insurance through his employer, he never utilizes any health care services. He often skips annual wellness visits as he says he “never gets sick.”  A few weeks ago, Yufei’s family noticed that he has been skipping meals frequently saying he’s full or not hungry. At his daughter’s urging, he decided to go for a visit. After conducting some more tests, his doctor explained that the chronic infection with the hepatitis B virus had progressed substantially, and he had developed cirrhosis. After an MRI diagnosis, it was revealed that Yufei had liver cancer
A few weeks ago, Yufei’s family noticed that he has been skipping meals frequently saying he’s full or not hungry. At his daughter’s urging, he decided to go for a visit. After conducting some more tests, his doctor explained that the chronic infection with the hepatitis B virus had progressed substantially, and he had developed cirrhosis. After an MRI diagnosis, it was revealed that Yufei had liver cancer The Hepatologist (liver doctor) explained to Yufei that the liver is an important organ and acts as a cleaning system for the body. It removes toxic waste, purifies blood, and helps to digest food properly. When the virus entered the liver, it made many copies of itself and started attacking healthy liver cells. This led to inflammation and weakened the ability of the liver to carry out its most essential tasks. Because he was never monitored for hepatitis B, the virus allowed tumors to grow in the liver which caused the cancer. When the tumors grow in size or number, it eventually spreads to other parts of the body and disrupts other vital processes as well.
The Hepatologist (liver doctor) explained to Yufei that the liver is an important organ and acts as a cleaning system for the body. It removes toxic waste, purifies blood, and helps to digest food properly. When the virus entered the liver, it made many copies of itself and started attacking healthy liver cells. This led to inflammation and weakened the ability of the liver to carry out its most essential tasks. Because he was never monitored for hepatitis B, the virus allowed tumors to grow in the liver which caused the cancer. When the tumors grow in size or number, it eventually spreads to other parts of the body and disrupts other vital processes as well. The doctor mentioned that liver cancer is often called the silent disease because symptoms may not always be present. Even with a hepatitis B, a person could look or feel okay but that does not mean the virus isn’t active and causing damage. When the symptoms do show up, it might be too late to prevent liver cancer. After discussing his options with the doctor, Yufei learned that the best treatment for him was to get a liver transplant.
The doctor mentioned that liver cancer is often called the silent disease because symptoms may not always be present. Even with a hepatitis B, a person could look or feel okay but that does not mean the virus isn’t active and causing damage. When the symptoms do show up, it might be too late to prevent liver cancer. After discussing his options with the doctor, Yufei learned that the best treatment for him was to get a liver transplant.