There are many misconceptions about the hepatitis B virus. One recurring one is the myth that hepatitis B is a genetic or hereditary disease. The belief is that because multiple family members can be infected by hepatitis B, it must be a virus that runs in families. This is not true. Hepatitis B is NOT genetic. Hepatitis B is spread through direct contact with infected blood. Although transmission can occur a number of different ways, it does not happen at conception or while the child is developing in the uterus.
Let’s start by breaking down what it means for something to be genetic or hereditary:
A genetic disease is caused by an error in a person’s genes and is carried by an individual in their genes. This type of disease may be passed on to a person’s child (which means it is hereditary) or it can occur spontaneously as a result of a gene mutation while a child is growing in the womb. Genes – which make up each of our unique DNA strands – are passed on to a child from both the mother and the father. Therefore, if a mother or father carries a certain hereditary disease or genetic trait, such as brown hair or green eyes, the child has the ability to have that as well.
Hepatitis B is not a genetic disease because it does not exist in a person’s genes. It is not carried in the egg of a woman or the sperm of a man. The hepatitis B virus exists in the liver cells and circulates in the bloodstream. Unlike a genetic disease, a person is not born with the hepatitis B virus already in their bodies. Instead, the virus is passed from mother to baby during childbirth through infected blood passing from the mother to the child during the physical delivery process. If a pregnant woman tests positive for hepatitis B, she can pass the virus to her newborn through infected blood and tiny tears in the skin that occur during childbirth. Oftentimes, these tears are unable to be seen by the human eye but can still allow for the virus to pass through and make direct contact with mucous membranes (“wet skin”) of the eyes, ears, nose, and mouth of the infant
A number of different factors play a role in determining if a newborn will contract hepatitis B from their mother: the mother’s viral load levels, the mother’s knowledge of her infection, and if the newborn receives post-exposure prophylaxis. Post-exposure prophylaxis is the key to preventing mother-to-child transmission and consists of two parts: the first dose of the hepatitis B vaccine and hepatitis B immunoglobulin (HBIG). Both shots need to be administered 1) in two different limbs and 2) within 12 hours of birth in order to be as effective as possible. Once the shots have been given, the infant should complete the standard hepatitis B vaccine schedule in order to ensure that they are protected for life! *Please note that HBIG is not recommended by WHO, so it may not be recommended or available in all countries.
Commonly Asked Questions:
It can be difficult to understand facts when they do not align with what you have been told for many years, so we’ve answered some of the most common responses to our information below:
- If it is not genetic, how is it sexually transmitted?
This question goes back to the topic of genes. A genetic disease differs from a sexually transmitted disease because of where the virus is hosted during transmission from one individual to another. A genetic disease is given to a person via cellular DNA while a baby is developing in the mother’s womb. Sexual transmission occurs because the virus is present in blood and sexual fluids and can be transmitted through very tiny, microscopic tears as a result of sexual intercourse.
2. If it’s not genetic, why do multiple members of my family have it?
Families tend to share objects – and that’s okay! However, sharp objects like earrings and body jewelry or personal care items like razors, nail clippers, or toothbrushes, can make tiny, microscopic cuts and abrasions in our skin that bleed. Sometimes, we don’t even notice! When a family member uses an object with trace amounts of infected blood and they also have a wound, such as a mouth sore, cut, or freshly shaved skin, the virus can spread to the uninfected individual. Because hepatitis B is so infectious (at least 50 times more infectious than HIV!), even small amounts of infected blood can cause a person to become infected. Therefore, it is recommended that personal items and sharp objects are not shared – even between family members, or ensure all family members are properly vaccinated for hepatitis B and confirm they are protected
Accidents also occur frequently in households, and sometimes blood is spilled. The virus can live on surfaces outside of the body, so it is essential to properly clean up any blood spills. The key to safely cleaning up blood and killing the virus is to wear gloves and use a fresh diluted bleach solution of 1 part bleach mixed with 9 parts water.
It’s extremely important to note that infected blood must come into contact with uninfected blood or a mucous membrane for transmission to occur. A person cannot become infected from skin-to-skin contact such as shaking hands or hugging, sharing utensils or food prepared by an infected individual, or even kissing.
Prevention:
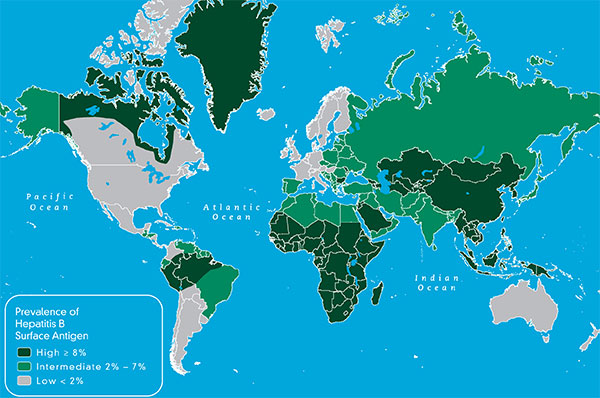
The best thing to remember is that hepatitis B is preventable, even if a child is born to a mother living with chronic hepatitis B! Always remember to wash your hands thoroughly with soap and hot water after any possible exposure to blood. In addition, any family members and loved ones who test negative for the hepatitis B surface antigen (HBsAg) and did not recover from a past infection (HBcAb total negative) should get vaccinated to prevent any possible transmission. The vaccine is one of the most effective vaccines in the world!


 On the other hand, hepatitis B begins as a short-term infection, but in some cases, it can progress into a chronic, or life-long, infection. Chronic hepatitis B is the world’s leading cause of liver cancer and can lead to serious liver diseases such as cirrhosis or liver cancer. Most adults who become infected with hepatitis B develop an acute infection and will make a full recovery in approximately six months. However, about 90% of infected newborns and up to 50% of young children will develop a life-long infection. This is because hepatitis B can be transmitted from an infected mother to her baby due to exposure to her blood. Many infected mothers do not know they are infected and therefore cannot work with their physicians to take the necessary
On the other hand, hepatitis B begins as a short-term infection, but in some cases, it can progress into a chronic, or life-long, infection. Chronic hepatitis B is the world’s leading cause of liver cancer and can lead to serious liver diseases such as cirrhosis or liver cancer. Most adults who become infected with hepatitis B develop an acute infection and will make a full recovery in approximately six months. However, about 90% of infected newborns and up to 50% of young children will develop a life-long infection. This is because hepatitis B can be transmitted from an infected mother to her baby due to exposure to her blood. Many infected mothers do not know they are infected and therefore cannot work with their physicians to take the necessary