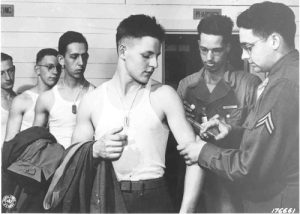
With Veterans Day comes reports about the lack of adequate mental health care for men and women returning from war. There is another, invisible health issue threatening veterans of all ages–hepatitis B.
Few veterans have ever been screened or treated for hepatitis B though their infection rate is four-times the national average.
The percentage of veterans infected with hepatitis B may actually be higher, but no one knows. Only 15 percent of U.S. veterans have ever been screened for hepatitis B. Among the few screened and diagnosed with chronic hepatitis B, only 25 percent have received antiviral treatment and only 13 percent have been screened for liver cancer. Continue reading "The Veterans Administration Ignores an Enemy on the Homefront: Hepatitis B"



