HBF is pleased to connect our blog readers to Christine Kukka’s monthly HBV Journal Review that she writes for the HBV Advocate. The journal presents the
latest in hepatitis B research, treatment, and prevention from recent academic and medical journals. This month, the following topics are explored:
HBF is pleased to connect our blog readers to Christine Kukka’s monthly HBV Journal Review that she writes for the HBV Advocate. The journal presents the
latest in hepatitis B research, treatment, and prevention from recent academic and medical journals. This month, the following topics are explored:
- Belatedly, National Panel Recommends Screening At-Risk Patients for Hepatitis B
- Genotypes and Mutations Define the Course of Hepatitis B Infection
- Older Patients Who Lose HBeAg After Treatment May Relapse
- Tenofovir Proves Ineffective in Patient with Multiple Drug Resistance
- Nearly All HBeAg-Negative Patients Relapse After Antiviral Treatment Stops
- Studies Find Hepatitis Infection Does Not Increase Pancreatic Cancer Risk
- Screening Pregnant Women for High Viral Loads Is Cost Effective
- Hepatitis B Appears to Impede Fertility
- Despite Low Viral Load, Infected People Can Still Infect Family Members
- Good News: HBV Infection Rates Lower Than Expected Among Korean-Americans
- Green Tea May Be an Effective Antiviral
HBV Journal Review
June 1, 2014
Volume 11, Issue 6
by Christine M. Kukka
Belatedly, National Panel Recommends Screening At-Risk Patients for Hepatitis B
Ten years after it recommended against screening the “general population” for hepatitis B, an independent national task force that creates prevention guidelines for primary care providers has finally recognized that certain high risk groups in the U.S. should be screened for hepatitis B.
Their recommendations, recently published in the Annals of Internal Medicine, come after numerous studies faulted primary care providers for failing to screen patients for hepatitis B and missing opportunities to treat patients for liver disease and immunize family members against hepatitis B virus (HBV) infections.
Other health care organizations, including the U.S. Centers for Disease Control and Prevention (CDC), the Institute of Medicine, and the American Association for the Study of Liver Disease, have been recommending for years that primary care doctors screen high-risk patients for hepatitis B, which has infected up to 2.2 million Americans.
The U.S. Preventive Services Task Force (USPSTF) recently issued clinical guidelines recommending that doctors screen the following patients for hepatitis B:
- People from countries that have hepatitis B rates exceeding 2% (which includes Asia, Africa, Central Europe and parts of Central and South America).
- U.S.-born people whose parents immigrated from countries with high rates of HBV infection.
- HIV-positive people, injecting drug users, men who have sex with men, and
- Household contacts of people infected with HBV.
The task force’s guidelines suggest that because an effective vaccine to protect against the infection and effective treatments for hepatitis B are now available, they decided to issue these recommendations. However, both the vaccine and effective treatments have been available for more than a decade.
“In the 2004 recommendation, the USPSTF focused only on the general population,” the authors wrote in the recommendations. “In the current recommendation, the USPSTF focused on high-risk populations as it considered new evidence on the benefits and harms of antiviral treatment, the benefits of education or behavior change counseling, and the association between improvements in intermediate and clinical outcomes after antiviral treatment.” The task force noted that it, “…found inadequate evidence that education or behavior change counseling reduces disease transmission.”
Source: www.uspreventiveservicestaskforce.org/uspstf/
uspshepb.htm
Genotypes and Mutations Define the Course of Hepatitis B Infection
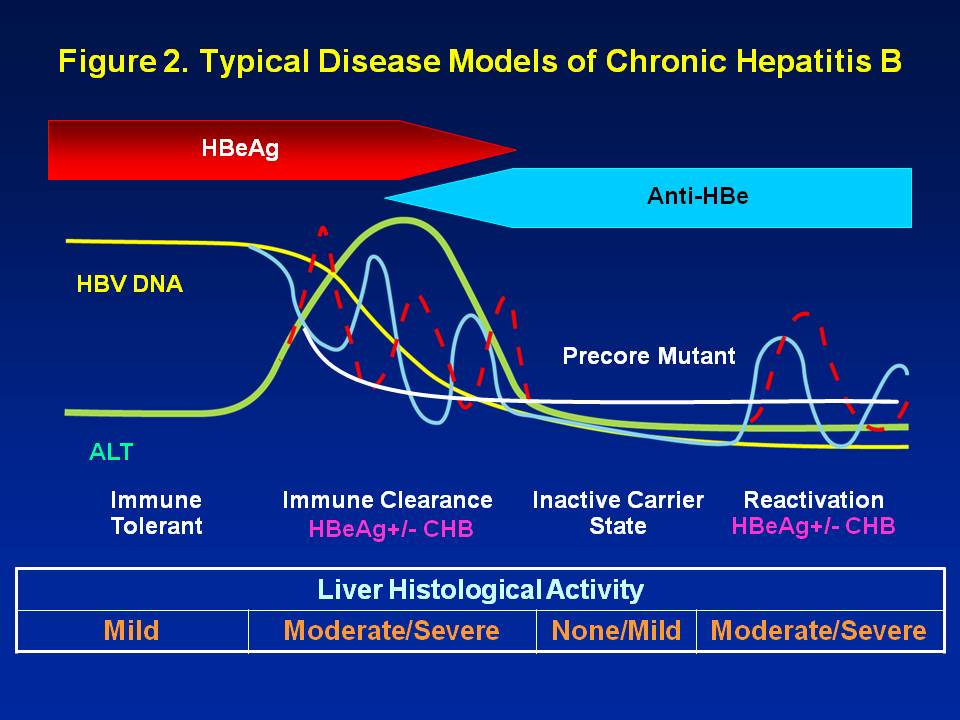
Researchers are increasingly finding that HBV genotypes or strains—and the mutations that they generate—can determine the severity of a patient’s infection.
Each of the world’s 10 genotypes and their mutations have different characteristics that can increase risk of cirrhosis and liver cancer, determine whether an infection becomes chronic, and basically determine a patient’s destiny, according to a recent study, published in the May issue of the World Journal of Hepatology …
Continue reading the HBV Journal Review…