
B Heppy Recap: A Global Perspective on Stigma and Discrimination Against Hepatitis B
Catherine Freeland is the Associate Director of Public Health Research at the Hepatitis B Foundation. As a researcher and founder of the Foundation’s Hepatitis B Discrimination Working group, Dr. Freeland shares more about the impact of discrimination and stigma as it pertains to people living with hepatitis B.
What is the difference between stigma and discrimination?
- It’s important to understand stigma and discrimination are different. Stigma is a social process that is characterized by being excluded, rejected, and devalued because of the social judgement associated with a certain condition. Although the literature on the topic is limited, it has been shown that stigma related to hepatitis B has negatively impacted the quality of life for those living with hepatitis B around the globe. Discrimination is different in that it is characterized by the laws and behaviors that limit opportunities for growth. For example, denying access to education or work because someone is living with hepatitis B is a form of discrimination. Discrimination is often a result of stigma.
What are the causes for stigma and discrimination as it pertains to hepatitis B?
- Lack of knowledge and understanding about hepatitis B in the community is a root cause of stigma and discrimination. Most people are unaware of what hepatitis B is and how it can be transmitted. This often results in rumors, myths and misconceptions spreading in the community and unfortunately can alienate people living with hepatitis B.
How does stigma and discrimination against hepatitis B affect the lived experiences of people in the community?
- When myths and misconceptions spread about hepatitis B in the community, people with lived experience often face discrimination. A lot of people are required to undergo health screenings prior to starting employment. If they test positive for hepatitis B, they can be denied employment and/or can be fired from their jobs in many parts of the world. It can then be difficult to find another job and support their families. For people who wish to get employment visas to work abroad, they are required to undergo health screenings. In the Philippines and the Gulf Coast (Bahrain, Kuwait, Oman, Qatar, Saudi Arabia and the United Arab Emirates countries), it is common practice to deny employment visas to people living with hepatitis B. In some countries and cultures, pre-marital screening. We have also heard cases of individuals living with hepatitis B experience more challenges in custody of their children in divorce or separation cases.
How can we address these challenges and what is the Foundation doing to support people experiencing discrimination?
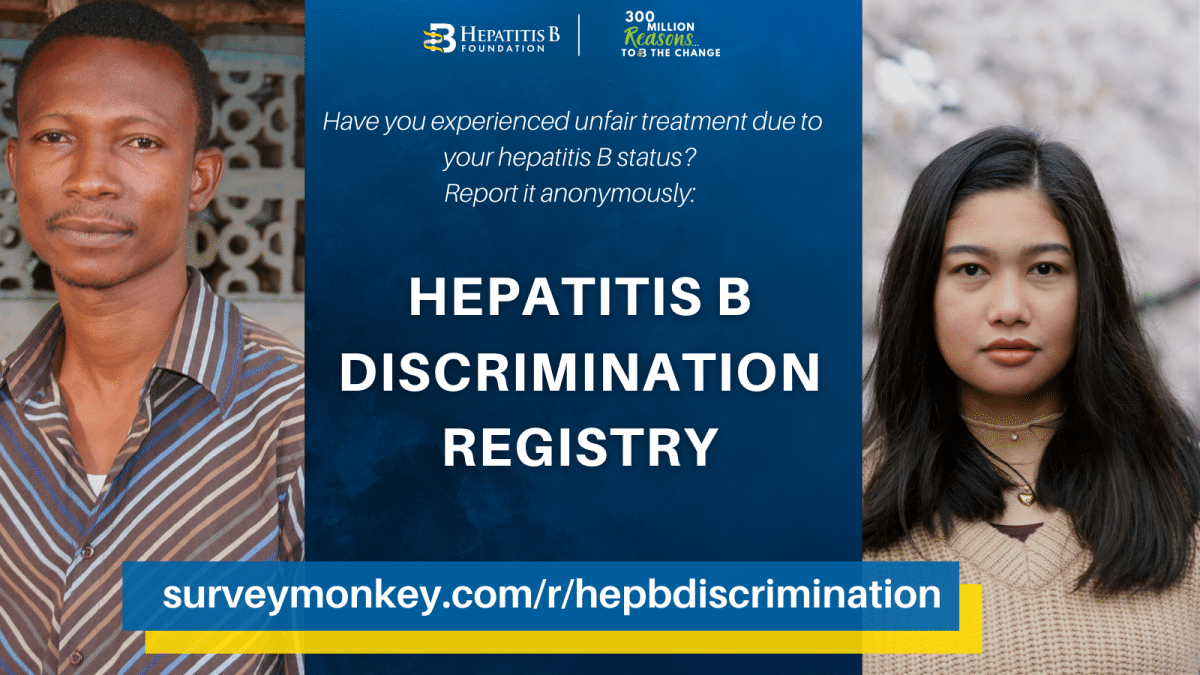
- It is important for people with lived experience to speak up and share their experiences of stigma and discrimination. At the Hepatitis B Foundation, we have a discrimination registry where people can fill out survey responses pertaining to any discrimination, they are facing in their home countries. The survey is free and open access. We also have a working group of experts consisting of people with lived experience and community leaders and partners. By raising awareness about discrimination, we are working towards changes in policy across the globe to reduce stigma, improve lives, and give people living with hepatitis B a voice that matters. Ultimately everyone has a role to play in addressing discrimination and it starts with education and sharing accurate information on hepatitis B and advocating against this discrimination and stigma.
Listen to the full episode here!


 Hepatitis B and Stigma
Hepatitis B and Stigma 
 Around the world, millions of people with chronic hepatitis B face wrenching discrimination that limits their dreams, education, careers, income and personal relationships.
Around the world, millions of people with chronic hepatitis B face wrenching discrimination that limits their dreams, education, careers, income and personal relationships.
 This military code historically barred people with serious medical conditions because they were considered unfit to serve, suspected to incur high healthcare costs and could pose an infection risk to fellow soldiers.
This military code historically barred people with serious medical conditions because they were considered unfit to serve, suspected to incur high healthcare costs and could pose an infection risk to fellow soldiers.