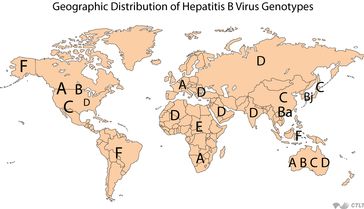
 Below is a publication from “Healio Hepatology, January 23, 2013 –HBV Genotype C Carries Greater Risk for HCC Than Other Genotypes“, showing the risk of hepatocellular carcinoma among the different hepatitis B genotypes based on a meta-analysis of 43 studies. There are 8 identified HBV genotypes ranging from genotypes A through H. These different genotypes are concentrated in distinct geographic areas of the globe, and may influence the course of disease, as noted below with the greater risk of liver cancer for those with genotype C.
Below is a publication from “Healio Hepatology, January 23, 2013 –HBV Genotype C Carries Greater Risk for HCC Than Other Genotypes“, showing the risk of hepatocellular carcinoma among the different hepatitis B genotypes based on a meta-analysis of 43 studies. There are 8 identified HBV genotypes ranging from genotypes A through H. These different genotypes are concentrated in distinct geographic areas of the globe, and may influence the course of disease, as noted below with the greater risk of liver cancer for those with genotype C.
Patients with hepatitis B genotype C are more likely to develop hepatocellular carcinoma than patients with other HBV genotypes, according to recent results.
Researchers performed a meta-analysis of 43 studies (34 cross-sectional, four case-control, four prospective or retrospective cohort studies and one randomized controlled trial) published between 1999 and 2010 assessing the risk for hepatocellular carcinoma (HCC) across the major genotypes of hepatitis B.
Analysis included data on 14,545 patients with HBV, with 517 cases of genotype A, 4,417 of B, 7,750 of C, 1,506 of D, 57 with A and D in combination and 298 with other and/or mixed genotypes. There were 2,841 patients with HCC across all studies.
In 33 studies comparing genotypes B (n=4,417) and C (n=6,060), HCC was significantly more common among participants with genotype C (25% of patients vs. 12%), with an OR of 2.05 (1.52-2.76). Patients with genotypes A (n=517) and D (n=1,506) were at similar risk for HCC across 12 studies (14% for A vs. 11% for D, OR=0.94, 0.67-1.32). Patients with genotype C (n=1,659) were at significantly higher risk than those with genotypes A or D (n=1,403) in 10 studies (30% vs. 7%, OR=2.34, 1.63-3.34). Analysis of HBV subgenotypes Ce (n=1,440) and Cs (n=715) in eight studies indicated a similar risk for HCC between subgenotypes (OR=1.13, 0.76-1.67) (95% CI for all).
“Genotype C HBV is associated with a higher risk of HCC than genotypes A, B and D HBV based on studies largely observational,” the researchers wrote. “This partly explains a higher risk of HCC among patients in Southeast Asia where genotype C HBV is prevalent. Patients infected with genotype C HBV, which is often associated with more active liver disease and higher risk of liver cirrhosis, should be closely monitored for HCC development and considered for antiviral therapy.”
Disclosure: See the study for a full list of relevant disclosures.