Liver-friendly diets are a common concern for those with chronic hepatitis B wishing to make healthy lifestyle choices. Protein is essential to all, but there are healthier ways to consume necessary proteins. Please enjoy this informative blog from the Al D. Rodriguez Liver Foundation – ADRLF, on Protein Myths and Your Liver written by ToniMarie Bacala.
We all love need protein – whether it be from animals or plants—protein gives us essential amino acids we need to keep our bodies strong and healthy. But how much do we really understand about protein and its effects on our organs, especially the liver? Is there such as thing as too much protein, even if its from vegetables and grains? Let’s delve into two popular protein myths and how we can ensure our protein intake is safe for our liver.

Protein is made of 20 different amino acids, but only 11 of which can be naturally synthesized by our body. The other types of protein come from the food we eat. Essentially, it’s safe to say that while protein helps in building the cell wall, strengthening muscle tissues and supporting cell functions, our body actually just needs certain types of amino acids.
So myth or truth? The best source of protein is animal meat. MYTH
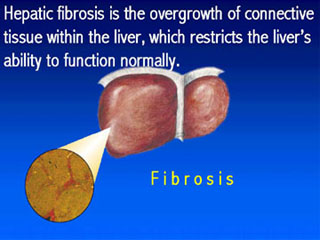
Eating red meat requires our digestive system, as well as our liver to do a lot of work processing the heavy bulk of protein. Experts suggest limiting the amount of red meat we eat to at most one serving a day.
There are other good sources of proteins like whole grains, green vegetables, nuts, peas and beans. Fruits also contain small amounts of protein. Compared to animal meat, vegetables and beans have phytochemicals, antioxidants and other nutrients. Nuts and beans containing antioxidants help the liver process the food and beverage that we take in, making it a healthier source of protein.
Myth or truth? People desiring to build lean muscle mass can eat as much protein-rich food as they want.
MYTH.
There is such a thing as too much protein. While protein is an essential nutrient, the overall health of our body lies in having a balanced diet. People building up muscles such as athletes and bodybuilders are no different.
The advisable amount of protein intake for men also differs from women. Consult your doctor or a nutritionist who can give you the appropriate amount of protein you should include in your diet, as based on your weight, age and daily activities. There are also vegan bodybuilders who get much of their protein requirements from vegetables and grains.
Eating too much protein can cause several health conditions such as ketosis, organ failure, and heart diseases. Too much protein can also be dangerous and stressful to the liver. So look out for other protein myths with the basic truth in mind: Keep protein intake in moderation and explore the benefits of non-animal sources of healthy proteins.